We created this toolkit because harm reduction programs are under-resourced and need additional funding — with the U.S. reaching 100,000 overdose deaths in the first year of the pandemic there is an urgent need for the healthcare system to fund work that is designed and driven by people who use drugs across the country.
National Harm Reduction Coalition, Vital Strategies, In The Works, and Anka Consulting partnered to produce the “Harm Reduction is Healthcare: Sustainable Funding for Harm Reduction Programs” toolkit because we’re committed to seeing harm reduction grow and thrive — and there is a unique opportunity unlike ever before to pursue healthcare financing. We’ve been leaders of harm reduction programs and know how exhausting the deliverable treadmill and precarious public health dollars can be. We created this toolkit because harm reduction programs are under-resourced and need additional funding — with the U.S. reaching 100,000 overdose deaths in the first year of the pandemic there is an urgent need for the healthcare system to fund work that is designed and driven by people who use drugs across the country. Not only is it possible to pursue healthcare financing in a way that doesn’t burden community-based harm reduction programs with administrative or billing logistics, but healthcare systems need harm reduction programs to partner with to close gaps on the continuum of care. This toolkit was designed for leaders of harm reduction programs and was conceptualized with the input of harm reduction leaders across the country.
This project was supported with funding from the Bloomberg Philanthropies Overdose
This interactive toolkit contains several components, all free to access for harm reduction programs and organizers. Please navigate to the button that reads “Download PDF” for a PDF of the workbook and the public drive of resources for all of these resources in layout, available to download free. This page is for full accessibility with all text on the page and image descriptions for all images.
90-minute Harm Reduction is Healthcare Course
Not sure how the healthcare system works? Staying too busy running a program to keep up with the many changes of the Affordable Care Act or Medicaid Expansion? Maybe you are clear, but you have team members who need a crash course so they can participate in conversations. We’ve got you covered. Take our free 90-minute e-course to refresh your memory, get on the same page about the language and systems, and get inspired by case studies from your peers.
This project was supported with funding from the Bloomberg Philanthropies Overdose Prevention Initiative
Harm Reduction is Healthcare: An Overview
After you’ve reviewed the e-course, download this simple handout with some key explanations to keep on hand for yourself or team members who are part of your assessment.
Harm Reduction is Healthcare: Glossary
Download this quick reference glossary of terms and processes that are commonly referred to throughout the e-course and in conversations about healthcare financing.
Harm Reduction is Healthcare: A Workbook for Harm Reduction Organizations
After you’ve taken the e-course for background, take time to reflect, plan, and act to pursue healthcare financing options that make sense for your organization. The workbook includes self-assessments, links to downloadable templates, and facilitator guides on how to work with your team and community to make choices about partnerships with healthcare entities or expanding your own health services. You can download the workbook PDF from our Public Drive or access a text-on-page web version of the workbook here for full accessibility.
Vital Strategies, Quinnipiack Valley Health District, Public Health Program Assistant, New Haven, CT 2021
Whether you’re new to healthcare financing or have tried and didn’t get anywhere, we know that being on the deliverable treadmill is tiring and the dollars aren’t always reliable. This self-assessment tool is for leaders of harm reduction programs who are looking for guidance on how to internally and externally assess opportunities to pursue healthcare financing for their program.
- Introduction
- Step 1: Learn & Review the Basics of Healthcare Financing
- Step 2: Organizational Readiness Assessment
- Step 3: Mapping Out Billable Services
- Step 4: Mapping Out What It Takes to Get People to Services
- Step 5: Creating Your Organization’s Value Proposition
- Step 6: Choose Your Healthcare Financing Adventure
- Step 7: Mapping Out Potential Partners
- Step 8: Setting an Agenda
- Step 9: Organize & Advocate
- Acknowledgments
- Appendices
National Harm Reduction Coalition & Vital Strategies partnered to produce the “Harm Reduction is Healthcare: Sustainable Funding for Harm Reduction Programs” toolkit because we’re committed to seeing harm reduction grow and thrive — and there is a unique opportunity unlike ever before to pursue healthcare financing. We’ve been leaders of harm reduction programs and know how exhausting the deliverable treadmill and precarious public health dollars can be. Not only is it possible to pursue healthcare financing in a way that doesn’t burden your organization with administrative or billing logistics, but the healthcare systems need harm reduction programs to partner with to better close the gaps on the continuum of care. This toolkit was designed for leaders of harm reduction programs and was conceptualized with the input of harm reduction leaders across the country.
Introduction
Foreword by Dr. Kima Taylor

The overdose crisis, COVID-19, budget cuts, racial justice, and the counter-protests have created opportunities for the inclusion of high-quality culturally relevant harm reduction services. The opioid overdose crisis opened the door to public health and health care systems to even consider harm reduction, but this was predominantly because the opioid overdose crisis was thought to reside within white communities; communities that were deemed unexpendable. COVID-19 made policymakers finally see longstanding racial and ethnic health and economic inequities within our systems, the murders of George Floyd, Breonna Taylor, and Duante Wright and the subsequent protests have forced sustained attention towards rethinking the country’s racist past and policing. Budget cuts following COVID-19 will place even more urgency on for health care systems to find savings and/or contain costs, ultimately leading to expanded pay for value programming. This systemic churn offers a small window of opportunity for harm reduction providers to engage in partnerships with health care payers that would provide comprehensive sustainability funding.
While foundation and state block grant funding will always be an appreciated and important part of most Syringe Service Programs (SSPs) and other harm reduction service provider budgets SSPs are well suited to pursue a health care financing strategy as well. SSP’s services benefit social, health, and public health system clients as well as those systems’ bottom lines. Many physical health care payers and providers have little to no ability, or history, of effectively working with and engaging people who use drugs. Case management, care coordination, outreach, engagement, public health screening, physical health and substance use services at SSPs offer connection and services to communities and people who health systems have refused to engage in the past. Prior to the Affordable Care Act (ACA) their clients were uninsured and deemed costly and less valuable by the health, public health, and justice systems. Following the ACA, many clients have Medicaid or other insurance, and payers are now financially responsible for their health.
History has long demonstrated that merely having coverage is not the same as receiving respectful, high-quality, culturally and linguistically effective care that leads to equitable outcomes. The powerful health care system is rife with example of inequities; most recently maternal child health mortality and morbidity is in the news; this is just one example of inequitable outcomes based on race and ethnicity. Sustainable funding for harm reduction will require a deconstruction of health care system racism and bias towards people who use drugs. It will require diverse advocates of all types, including those who are currently using drugs, to hold the health and public health systems to account to ensure equitable access to and outcomes from services; lest this endeavor be yet another system where white people will benefit and others will not.
This work is complex and can seem exhausting but is not impossible. The guide is not meant to obscure the work needed to accomplish the goal, but to provide guidance to make that work a bit easier, effective, and includes a racial justice lens. The goal of the brief is also to promote a new type of engagement, not the fee-for-services pathway which while rewarding in some places is not the current wave in health care financing. The new wave is focused on payment for equitable holistic outcomes with an eye (sometimes with a principal goal) of creating cost savings. It is with this lens the guide provides guidance for engagement.
Pursuing a financial sustainability strategy with an outcomes-based lens requires SSPs to define their mission as it relates to health care relationships, define their work, cost the services out, and be able to articulate their value proposition in health care terms. Value proposition in hand, they must next identify which health care players offer the best reciprocal benefits and educate these potential partners about harm reduction services ultimately seeking beneficial contracts. During the identification phase, SSPs need to carve out time to meet new players, understand their motivations and concerns, and build advocacy and content partners. So much of health care policy, practice, and programming is based on relationships.
At the same time, SSPs must remain somewhat cautious. The same events that have opened a window are also leading to unrealistic expectations or smaller organizations not fully benefiting. People want easy answers for complicated situations. SSP’s must be sure not to overpromise in such an environment or they will lose their credibility and ultimately the funding. Harm reduction programs should exercise caution when promising returns on investment or changes in community health curves; they should likely start with cost containment and individual health engagement and improvements. They must make sure they identify short, medium- and long-term process and health outcome measures so they are not judged solely on their ability to get people to enter treatment.
An equity lens means recognizing the strengths and shortfalls of your program in addressing the needs of BIPOC, undocumented, LGB/TGNC+, disabled, and otherwise marginalized participants. These groups are not monoliths, and promising to meet the needs of all communities is unrealistic, sets your organization up for failure, and leaves communities without access to high-quality services. SSP’s should also lead with an equity lens but should not pretend they can serve all populations with one model. If they have a history of providing culturally effective services to diverse communities they should lead with this accomplishment. If not, they should take the time to learn how or recommend other service providers.
The past two years have been painful in so many ways, but opened the eyes of many to longstanding racism, inequities and injustices within our government funded systems. Patient-centered and culturally effective harm reduction organizations must take this time of turmoil to create financially sustainable relationships with health care and other systems that will lead to improved outcomes and help individuals thrive.
The purpose of this tool is to…
- (Re)consider how building new or different types of relationships with healthcare entities is a worthwhile endeavor to create sustainable funding and partnerships for years to come
- Create a value-proposition that outlines the value of the services your organization offers using healthcare language
- Guide conversations with key community stakeholders in your organization to assess the opportunities, potential drawbacks, and roles people need to take to move forward
- Create an action plan to build relationships with potential healthcare partners that can lead to healthcare financing opportunities for your organization
Step 1: Learn & Review the Basics of Healthcare Financing
We heard from the community that in order to understand pathways for healthcare financing, you need to better understand how healthcare financing actually works. We’ve gathered and created some additional tools as a way to orient yourself to the system and options before exploring which ones may work best for your program.
- 90-minute Harm Reduction is Healthcare E-Course
- Harm Reduction is Health Care Overview (link to PDF, plain text version in Module 3 for full accessibility)
- Harm Reduction is Health Care Quick Reference Glossary (link to PDF, plain text version in Module 4 for full accessibility)
- Harm Reduction is Healthcare Templates — a public Google Drive with templates of the assessments and tools included in this workbook
- Medicaid Expansion in Your State: Since every state is slightly different in their rules and regulations around Medicaid expansion, we recommend that you bring yourself up to speed on details specific to your state using the Kaiser Family Foundation Medicaid Expansion interactive map.
- Tool for Organizational Self-Assessment for Racial Equity: This tool created by Coalition of Communities of Color can support your own self-assessment, so as you are navigating your value proposition, partnerships, and how to address inequity in access to health services, you’re keeping racial equity front and center.
Step 2: Organizational Readiness Assessment
Who should fill this out: The leader(s) of the organization who can see the 30,000 foot view across the organization in the areas of mission, programming, finance, community partnerships, and governance. For institutional memory, support, and leadership development, we encourage you to bring in mid-level managers early in the process to learn how these decisions get made and offer opportunities for input and buy-in up front.
Directions: Answer the following question with the numbers that best describe where your organization is in relation to the activities and structures listed below. Before you jump into this, think about what you may need to do with your team to define some of the terms and what it looks like to operationalize some of these values.
|
1 No and/or Doesn’t Exist |
2
Yes, it have done some work but it’s very limited and/or not operationalized |
3
Yes, we’re working on it but not our strongest area of work |
4 Yes, and it’s one of our strongest areas of work |
Mission & Values
- Do you have a written mission statement that accurately reflects the work that your organization does today?
- Do you have articulated value statements for how your organization approaches its work?
- Do you have an articulated racial equity statement on how your organization centers racial equity?
- Do you aim to serve individuals who are uninsured or underinsured?
- Do you aim to serve individuals who may have co-occurring physical or mental health conditions?
- Do you offer your services in locations or venues where there are people who may be disconnected from social and healthcare services? (e.g. tent cities/encampments, single-resident-occupancy hotels)
- Are you the go-to organization in your geographic area that offers low-threshold services for people who use drugs?
- Do you have a mechanism in place like a participant advisory board or consumer advisory board to get ongoing feedback from people who receive services?
Services
- Do you offer a space for people who use drugs to congregate?
- Do you offer a space for people who trade sex?
- Do you offer services specifically for people at other intersections of oppression? (e.g. LGBT, TGNC, people living with disabilities, non-English speakers, immigrants, pregnant or parenting people)
- Do you offer mobile-based services?
- Do you offer walkabout/street-based outreach-based services?
- Do you offer services-based outreach (e.g. outreach to emergency departments, re-entry programs, defenders offices, LEAD initiatives)?
- Do you have a community-level rapid response plan for overdose spikes?
- Do you offer preventative health services that can reduce negative health outcomes? (e.g. vaccines, syringes, naloxone, wound care supplies)
- Do you enroll folks in social service or healthcare benefits?
- Do you offer individual one-on-one services for case management?
- Do you offer individual one-on-one services for behavioral health counseling?
- Do you offer any one-on-one services for healthcare-specific health education? (e.g. not physical health services but discussion on how to reduce injection related infections, overdose prevention, etc)
- Do you offer any one-on-one services for healthcare-specific care coordination? (e.g. setting up medical appointments, locating specialists, going to provider appointments, coordinating prescription pick up or needs to external providers)
- Do you offer any one-on-one services for healthcare specific medical services? (e.g. HIV or hepatitis C testing, wound care and treatment of abscesses, PrEP)
- Do you offer any one-on-one services for medical treatment services? (e.g. general visits with an MD/PA/DO/NP, onsite hepatitis C treatment, buprenorphine, prescriptions, vaccines, COVID-19 testing, reproductive health services including but not limited to contraception, pap spears, Plan B prescriptions)
- Do you offer any group-level services for healthcare specific topics? (e.g. hepatitis C support groups, diabetes management groups, sexual assault support groups, trauma-informed groups)
Staffing
- Do you have adequate staff to serve the existing services during the current hours?
- Do you have existing medical or services billing staff? (e.g. billing and coding specialists)
- Do you have existing staff to manage data and reporting?
- Do you have existing staff to conduct QI and QA?
- Do you have existing staff to create and manage contracts with funders (healthcare payers, foundations, and government entities)?
- Do you have leader(s) in the organization who are familiar with and committed to building partnerships with healthcare entities?
- Do you have a leader(s) in the organization who have already or can map out potential healthcare entities to partner with to build relationships?
- Do you have a consultant or team member who can offer staff clinical supervision?
- Do you have any credentialed staff (e.g. peer credentialed staff like “certified recovery specialists”, LCSWs) to offer behavioral health services?
- Do you have any credentialed consultants (e.g. “certified recovery specialists”, LCSWs) to offer behavioral health services?
- Do you have any credentialed staff (e.g. MD, DO, NP, RN, PA, MA) to offer medical services?
- Do you have any credentialed consultants (e.g. MD, DO, NP, RN, PA, MA) to offer medical services?
Systems
- Do you collect socio-demographic data (age, race, ethnicity, gender) for individuals who access care coordination or one-on-one services outlined above?
- Do you document services that you provide as outlined above? (e.g. written charts, outreach forms, electronic health records)
- Do you currently use an electronic health record system?
- Do you currently have a system in place for tracking referrals for people to external services for healthcare, housing, job training, or other services?
- Do you have a system for reporting on contract deliverables to funders and/or health departments?
Relationships
- Are you already formally partnered (e.g. have an MOU and do bi-directional referrals with ongoing communication) with a healthcare clinic in your area?
- Are you already formally partnered (e.g. have an MOU and do bi-directional referrals with ongoing communication) with a hospital system in your area?
- Overall, are these partners mission-aligned, equity-focused, and effective?
- Does your organization sit on any existing community health committees (e.g. hospital community advisory board) with a local health system?
- Does your organization have any individuals on your board that are affiliated with a potential health system partner?
- Is your organization part of any coalitions or multi-organization grants with other healthcare providers or entities?
Sustainability – Thinking about the next 3-5 years…
- Do you anticipate any funding gaps following COVID-19 emergency funding you may have received?
- Do you have sufficient funding for your program to operate its existing hours and services?
- Do you have a balance of funding between government, non-government foundation/private grants, individual donors/donations, and fundraising that if one was cut significantly you would still be able to operate without major disruption?
- Have you expanded your services to keep up with the growing volume of participants seeking your services?
- Have you expanded your services to keep up with the type of services that are needed to offer more comprehensive care?
- Have you been approached to be acquired or merged with a larger organization in your area?
Reflection Questions
- What were the three domains above that had overall higher numbers and may be your organization’s strengths?
- What were the three domains above that had overall lower numbers and may be your organization’s limitations?
- Do you think that working with a healthcare entity could help strengthen your organization’s current limitations? How so?
Looking for organizational support and technical assistance? Add your name to the list and tell us a bit more about what you’re looking for. We will be reviewing responses in early 2022 and follow up via e-mail.
Sign up for FREE technical assistance here
Step 3: Mapping Out Billable Services
Directions: In the Harm Reduction is Healthcare E-Course, we described how many services that harm reduction programs offer that may be directly billable and/or valuable to healthcare systems in achieving their health outcome goals via value-based payments. Next, take a deeper dive into the services that you offer to clearly map out what you currently offer and what you could potentially offer with additional funding. Remember, this isn’t about determining the maximum amount your team could accomplish! This is about figuring out what is doable so that your organization has an idea of what is realistic. At the end of the day, you do not want to over-promise for services that you will not be able to fulfill. If you prefer to type in y our responses and share with others, click here to download the accompanying Google Document template.
| Services | Estimated Services per Month | Estimated Clients Served per Month | Currently Offer | Potentially Offer |
| Preventative Services | ||||
| Vaccines – Hepatitis A/B | ` | |||
| Vaccines – COVID-19 | ||||
| Vaccines – Flu | ||||
| Vaccines – Other | ||||
| Naloxone | ||||
| Other | ||||
| Home & Community Based Services (HCBS) | ||||
| Case Management- Support | ||||
| Case management – Care coordination | ||||
| Case management- Care navigator | ||||
| Enrollment in benefits | ||||
| Adult day services | ||||
| Engagement services | ||||
| Other | ||||
| Behavioral Health Services | ||||
| Psychosocial assessments | ||||
| Counseling – in-person | ||||
| Counseling – telehealth | ||||
| Support Groups | ||||
| Other | ||||
| Medical Services | ||||
| Wound care & treatment | ||||
| PrEP/PEP | ||||
| HIV testing | ||||
| HIV treatment | ||||
| Hepatitis C testing | ||||
| Hepatitis C treatment | ||||
| STI testing | ||||
| STI treatment | ||||
| Reproductive health wellness checks (e.g. birth control or Plan B Rx) | ||||
| Pap smears | ||||
| General well-care visits | ||||
| General labs | ||||
| Drug treatment – buprenorphine | ||||
| Other | ||||
| Other | ||||
| Other | ||||
| Other | ||||
| Peer Support Services provided by credentialed peer workers and may overlap with HCBS above, see your state guidelines | ||||
| General wellness & coaching specific to recovery | ||||
| In-person advocacy/navigation to appointments | ||||
| Support with enrollment in benefits | ||||
| Support with housing placement | ||||
| Support with job training | ||||
| Other | ||||
| Other | ||||
| Other |
Step 4: Mapping Out What It Takes to Get People to Services
You’ve mapped out the service categories you offer (or could potentially offer with additional funding/support) that fall into the billable services category. Whether or not you decide to pursue direct billing on your own, it’s helpful to have these services mapped out when you partner with healthcare entities. But we know that it takes a lot to actually get to services. Harm reduction programs have the trust, rapport, and the culturally and linguistically effective approach to work with people who healthcare systems are trying to reach.
Who should be at the table for Step 4: People on your team who are doing day-to-day outreach, drop-in center management, linkage to care, and/or case management are the second best to talk about what it takes to successfully navigate someone to a service from start to finish; the best people to talk to are people receiving services themselves. In this step, we encourage you to meet with both people who consume harm reduction services, and people who support that process, to get in touch with what it takes.
Directions: You will find facilitator guides for three different groups below: care coordination team members, people who receive services, and the leadership team who are making decisions about service expansion. We recommend that you carve out at least 90 minutes to have these conversations with each of the groups. Once you’re all in the same room for a discussion, share the purpose of the discussion and how it is related to the organizational work and decisions that you’re considering. We’ve offered time guidance to keep you on track with your discussion. See the Appendix below for the full facilitation guides.
Great! You’ve thought about your organizational readiness, the services you offer, and the experiences your team and consumers have with getting healthcare services. You’re ready to start framing your value proposition.
Step 5: Creating Your Organization’s Value Proposition
Value propositions are basically your pitch about what your harm reduction program offers that benefits the health system and community health outcomes at large. Harm reduction programs offer a huge value to health systems that are looking to offer consistent preventative healthcare to avoid high-cost treatment down the road.
Harm reduction programs are very often serving people who may have one or more of the following:
- Substance use and related potential adverse health outcomes (e.g. overdose risk, injection-related viral and bacterial infections)
- Substance use and potential to want to access drug treatment (e.g. buprenorphine, methadone, contingency management, cognitive behavioral therapy, motivational interviewing)
- Co-occurring chronic health conditions (e.g. chronic hepatitis, HIV/AIDS, high blood pressure, diabetes)
- History of repeat use of emergency health services for preventable incidents (e.g. endocarditis due to an untreated injection-related infection, overdose)
What does a value proposition entail?
- Telling the story of what services you are offering, to whom, why they are needed, and what are the outcomes.
- This assessment is more than just having a demographic list, though that is important as well; it is a deep dive on who is effectively served and where there may be need for improvement.
- Harm reduction programs should also lead with an equity lens but should not pretend they can serve all populations with one model; be specific to what you already know about disparities and how your organization works to address them.
- Example value proposition: Check out this powerpoint from Washington Heights CORNER Project and how they started to frame their value-proposition to New York Presbyterian Hospital, which resulted in co-located services, co-funded positions, and receiving payments directly from the healthcare system for wrap-around services.
Facilitated Guidance on Setting the Stage for Your Value Proposition
Themes for your Value Proposition: As the leader of a harm reduction program you probably already know a lot of the components of what will go into your value proposition, but you don’t know everything. This is the stage of this process where including stakeholders will be an entry point for buy-in early on to consider healthcare financing. We have included the following questions to ask community stakeholders as you begin to form your value proposition.
Who should be in this conversation: Executive leadership, board members, senior staff, care coordination staff; can be done as a series of meetings with the same group of people or an iterative process with different groups reviewing different pieces best suited to their area of expertise and governance.
Directions: Review the following section topics and look back on your notes from Step 4. This is a great opportunity as a leader of an organization to cross check your responses to the following questions with your team and community member’s expertise. You can download a Google Slides template if you would prefer to type in your responses and share with others here.
Mission & Values
- What does your organization aim to address in your community?
- What are your core strategic areas of work?
- What are your core organizational values?
- Who does your organization serve directly?
- How does your organization center racial justice & equity?
Services
- What services do we offer to the community that nobody else offers?
- What wrap-around services do we offer that are related to improving community health?
- What services do we link to other providers in the community?
- What partnerships do we already have with other providers in the community?
Staffing
- What does our team look like in terms of capacity and strengths to offer care coordination and linkage to services?
- What skills do we already have onsite to offer health promotion, behavioral health, and medical services?
- How do we conduct outreach and engagement with people we serve?
- How much time do we spend navigating insurance enrollment/”turning insurance back on” in our existing care coordination services?
- How much time do we spend working with people to enroll or re-enroll in other services? E.g. SNAP, WIC, disability insurance, unemployment, housing-related programs
- What other support or capacity do we need to offer care coordination?
Systems
- What data do we already collect from people who receive services?
- Are there services for which we don’t collect any data?
- Are there services for which we collect some data? What data?
- Are there services for which we need to collect data? What data?
- Can we disaggregate data? What do we know about everyone we serve vs. other specific people we serve because of what services they access?
- What services do we feel are crucial to continue to not collect identifying information?
- What systems do we already have in place to document and coordinate care services? What insurance or identification information are we already asking?
- What gaps do we already know exist in how we offer care coordination?
Culture
- How would you feel if we were sharing your/participant identifying information with a potential health provider? Clinic? Hospital system?
- What kinds of information feels okay to share?
- Are there times where you would feel more comfortable sharing information depending on what the situation was? For example, if you had an abscess vs. experienced an overdose?
- What would it mean to ask for people who receive services to share their insurance information with us?
- How does asking for identification or insurance information impact our approach to offering low threshold services? When is it appropriate to ask for this information?
- What would you want to know to be sure that your/clients’ privacy is protected?
Partnerships
- Do you have providers that we work with that you trust?
- Who do you trust?
- Who do you not trust?
- What values feel important to you/the organization in building partnerships with healthcare entities?
Framing Specifically for Healthcare Entities
If your local health system (e.g. hospital, FQHC) were in a room with you and wanted you to describe what your organization specifically can offer to…
- Improve the health of the community at large
- Reduce hospital admissions or acute care episodes
- Improve care coordination and linkage
- Improve management of chronic conditions
… what would you say?
Writing Out Your Value Proposition
You’ve spent time talking to community stakeholders and collecting a lot of data. Now that you’re immersed in the experience and values of your community stakeholders, let’s start to write out your value proposition.
Click here to download a Powerpoint template for creating your own value proposition presentation
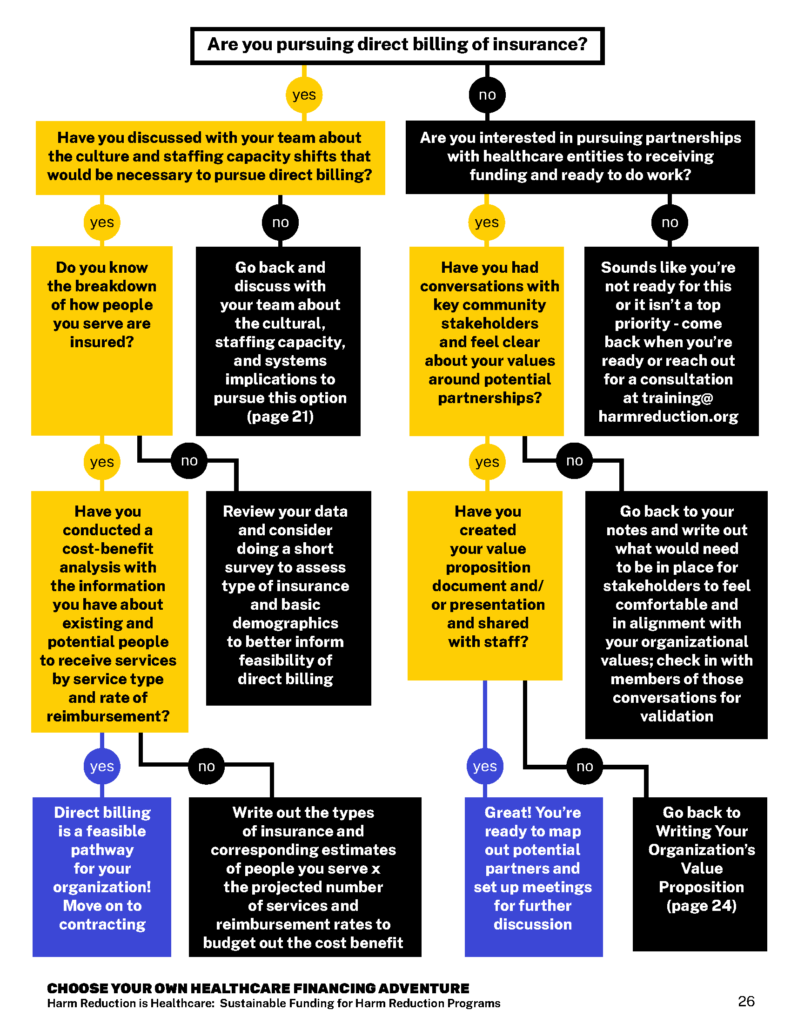
Step 6: Choose Your Healthcare Financing Adventure
You’ve been deep in data collection, service mapping, and creating a value proposition. The next step is to map out and build partnerships with potential partners – but let’s check that you’ve taken the steps to choose your healthcare financing adventure. This is a text description of a graphic flow chart (pictured below) available on page 26 in the full workbook version here.
-
- Are you pursuing direct billing of insurance? Yes / No
- If yes, have you discussed with your team about the culture and staffing capacity shifts that would be necessary to pursue direct billing?
- If yes, proceed to next yes
- If no, go back and discuss with your team about the cultural, staffing capacity, and systems implications to pursue this option (see page X)
- If yes, Do you know the breakdown of how people you serve are insured?
- If yes, proceed
- If yes, Do you know the breakdown of how people you serve are insured?
- If yes, have you discussed with your team about the culture and staffing capacity shifts that would be necessary to pursue direct billing?
- Are you pursuing direct billing of insurance? Yes / No
- If no, review your data and consider doing a short survey to assess type of insurance and basic demographics to better inform feasibility of direct billing
- If yes, Have you conducted a cost-benefit analysis with the information you have about existing and potential people to receive services by service type and rate of reimbursement?
- If yes — Direct billing is a feasible pathway for your organization! Move on to contracting.
- If no, Write out the types of insurance and corresponding estimates of people you serve x the projected number of services and reimbursement rates to budget out the cost benefit
- If no, Are you interested in pursuing partnerships with healthcare entities to receiving funding and ready to do work?
- If yes, proceed to next question
- If no, — sounds like you’re not ready for this or it isn’t a top priority, come back when you’re ready to reach out for a consultation at training@harmreduction.org
- If yes, Have you had conversations with key community stakeholders and feel clear about your values around potential partnerships?
- If yes, proceed
- If no, Go back to your notes and write out what would need to be in place for stakeholders to feel comfortable and in alignment with your organizational values; check in with members of those conversations for validation
- If yes, Have you created your value proposition document and/or presentation and shared with staff?
- If yes, proceed
- If no, Go back to Writing Your Organization’s Value Proposition
- If yes — Great! You’re ready to map out potential partners and set up meetings for further discussion
Step 7: Mapping Out Potential Partners
High-Level Mapping
You’ve collected a lot of data and created a value proposition so look back to your earlier notes from conversations with your team and community.
Let’s map them out to include the type of entity, name of the organization/entity, details of any existing relationship, overlap and areas for potential relationships, and next steps with contact information. We recommend doing this work with team members who offer care coordination services.
| Federally Qualified Health Centers (FQHCs)/Health Care for the Homeless Centers/Health Homes | ||||
| Name | Location(s) | Existing Relationship | Potential Relationship | Next Steps & Contact Info |
| Hospital Systems | ||||
| Name | Location(s) | Existing Relationship | Potential Relationship | Next Steps & Contact Info |
Do Your Research
After you’ve mapped out your potential partnership options, start doing some research. Here are some tips we have for you to begin to learn about each partner before you’re in the same room. In preparation for reaching out or connecting with individuals from healthcare entities, we recommend you do some of your own research.
Here are a few tips to feel confident going into that meeting:
- Review the healthcare entities website: note the language, types of programs that they feature on the front pages, and read their blog or news section to be up to speed on the kinds of work that is emerging, any health needs assessments they have (or haven’t!) done
- Review the healthcare entities partnerships: on their website or via a google search, note where the healthcare entity is partnering or sponsoring other community groups or causes in your neighborhood
- Review the potential partner’s provider list for services that overlap or touch folks who receive your services: get familiar with any of the providers who offer infectious disease, adult medicine, addiction medicine, and HIV and hepatitis C treatment
- Review how easy (or hard) it would be to make an appointment as a consumer: test it out as someone who has resources and make note of what was easy or difficult for you and how people you serve may experience the process. Note what you can bring to the table to make it easier.
- Review the organization’s statement or work related to racial equity: what is the organization doing to reduce disparities and address racial equity in their services? If this is missing, ask about it. If it’s not, dig in deeper to ask about how they’re addressing these inequities intersecting with stigma related to substance use specifically for people of color.
Step 8: Setting an Agenda
You’re almost there! You’ve done your research. You’ve talked with community stakeholders. You have your value proposition ready. And you have some partners you’re going to connect with next. But what do you talk about? Here are some suggestions for an agenda.
Preparation & Setup
- If you have space, bring them to your site. Don’t shut down your drop-in center because you want to impress your potential partner. Keep it real. This is an opportunity to connect the dots of what your program actually does since it’s possible they’ve never been to a harm reduction program.
- Give them a tour (in person or in photos) of where you offer services and where you conduct engagement. You want potential partners to be able to imagine where your (potential) overlapping services and clients are as a way to see how you’re already working in partnership, but just not in coordination. If you envision them coming and working in your site, show them where they would be and how it would work.
- Introduce them to your team! Prep any of your team members who will be part of the meeting and give them specific areas of the agenda that they can be the content expert and play a role in the meeting. Potential partners are looking at longevity and institutional memory – building these relationships and visibility of people doing the work is great leadership development and gives a nod to commitment.
Suggested Items for Discussion
- Introductions of all team members of your organization & the potential partner organization – names, pronouns, roles, how long they’ve been at the organization, and how familiar people are with each others work
- Orientation to a (brief) history of your organization – when it was founded, how it has grown, the values that you center including racial justice and equity – and why you reached out to the potential partner
- Ask the potential partners to share why they were open to meeting – what have they known about to date of your organization? Do they know any colleagues or people who have received services?
- What is the healthcare entity seeing in terms of people who may be accessing harm reduction services? Are they seeing a lot of injection related infections? Overdoses? What are they offering already?
- Share more about your approach to care coordination, case management, and general services here
- Share your value proposition
- What opportunities are there for collaboration? Do they have any specific initiatives related to overdose prevention or other areas of overlap? Need for additional linkage to care and wrap-around services?
- What are the next steps to formalize our partnership? What opportunities are there for participating in initiatives and being funded for coordinated wrap-around services? Who are the decision makers?
- Are there other forums, meetings, or people that your organization should be in contact with?
Step 9: Organize & Advocate
We’re calling this Step 8 but it’s really a necessary and parallel process. Every state is so different in terms of what is available, how regulations work, and available funds. And it’s people at the state or local government level that dictate how and if regulations are adopted for what services are valued. There is power in numbers so get a seat at the table. Here are a few tips to get started.
Read Up On Your State
- Do your research to understand what Medicaid expansion has looked like in your state – warm up your fingers and google keywords like Medicaid Expansion and value-based payments + your state name
- Look up the departments of health and substance use authorities to understand the bigger structures (if you don’t know this already)
- Read up on the carve ins / carve out structures in your state for behavioral health services, pharmacy programs, and other benefits offered in your state
- Map out the major managed care organizations and see if you recognize them as insurance that your participants have
- Talk to your contacts at the municipal/local, county, and state health departments to understand where funds are flowing since they may have higher-level insight – and take the opportunity to remind them that they should be on top of this for opportunities for harm reduction programs!
Organize Harm Reduction Programs
- Connect with other harm reduction programs (if you aren’t already) about health care financing opportunities and learn what others in your state are already doing
- Consider going through a process to map out your collective impact and services if you want to negotiate as a larger coalition/group/consortium
- Create a strategy together to map out the largest healthcare entities/organizations to organize meetings as a starting point of building a collaborative relationship that could lead to contracting and funding opportunities
Get a Seat at the Table
- Identify other places where you can take a seat at the table for harm reduction – including opportunities to be on task forces, working groups, offering public comment, and other places where there are decision makers in the room
- Talk about the value of harm reduction loud and proud at…
- Webinars organized by public health departments on general public health topics
- Community board meetings where there are usually representatives from health clinics and hospitals
- Conferences or meetings on general community health, healthcare, public health, health equity, addiction, or anything labeled “community engagement” “reaching hard to reach groups” etc
- Public testimony at city hall or capitol hill on legislation specific to insurance or treatment for people who are unhoused, using substances, etc
- Health and community assessment efforts driven by State and county health agencies, and/or local hospitals and public health entities which often include focus groups, public polls, stakeholder meetings, and/or surveys
- Check out the Pennsylvania Department of Health Statewide Health Assessment here
To learn more information about healthcare financing and support, you can visit:
- Anka Consulting LLC
Acknowledgements
Authors
Taeko Frost, DrPH, MPH
Kima Taylor, MD, MPH
Dana Kurzer-Yashin
Daliah Heller, PhD, MPH
Tracy Pugh, MHS
Graphic design by Andrea Marcos
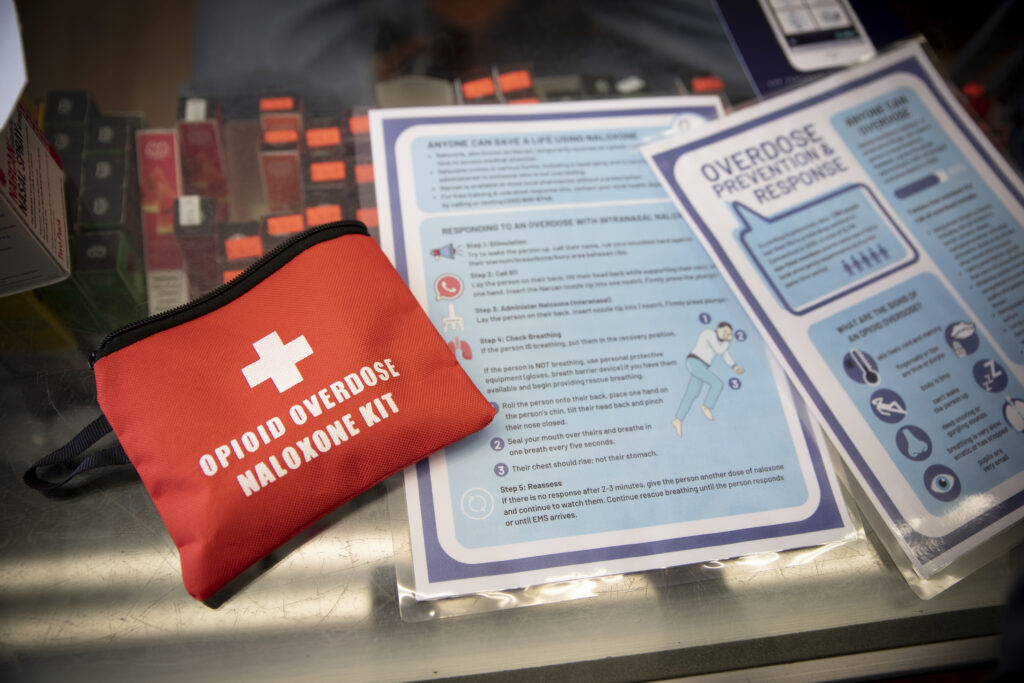
Photos provided by Vital Strategies’ Overdose Prevention Program and photographer Graham MacIndoe. These photos are part of the photo documentary series highlighting harm reduction titled “Love & Dignity: Portraits From the Front Lines of the Overdose Crisis.”
Appendices
Appendix A: Glossary
- Affordable Care Act (ACA) = the comprehensive healthcare reform law enacted in 2010 that expanded the number of people who could get insurance, expanded Medicaid in some states to make more people are eligible, and shifted the value to prioritize quality, access, and cost containment
- BIPOC = Black, Indigenous, and people of color
- Federal poverty level (FPL) = measure of income issues every year by the Department of Health and Human Services (HHS) and determine eligibility for certain programs and benefits such as Medicaid: see here
- Medicaid = a federal-state insurance program that services low-income individuals of all ages with zero to low co-payments.
- Medicaid expansion = expanding the eligibility of people who are eligible for Medicaid widening the income qualifications so that more low-income individuals and families are eligible to receive coverage under Medicaid.
- Medicare = a federal insurance program that serves people over the age of 65, as well as some younger people living with disabilities.
- Dual-eligible = people who are eligible for Medicaid (because of their income) and Medicare (because they are 65 or older and/or disabled).
- Healthcare entity = a provider, clinic, insurance company “payer,” or hospital system that offers healthcare services.
- Federally Qualified Healthcare Clinics (FQHCs’) = Federally funded to provide primary health care, social, and some specialty services to uninsured and underinsured populations, regardless of documentation. These clinics are required to serve folks, regardless of documentation, though historically they have not always been held accountable to this mandate. who are undocumented, but historically they have not honored this mandate.
- Behavioral health= the promotion of mental health, resilience and wellbeing; behavioral health services may include the treatment of mental and substance use disorders and supportive services for people who are receiving services and their caregivers. Read more about behavioral health services here.
- Accountable Care Organizations (ACO’s) = a highly integrated system of providers who share patients as a way to better offer comprehensive, coordinated care for each patient
- Managed Care Organizations (MCO’s) = a healthcare company or a “health plan” that is focused on managing the overall healthcare of individuals as a model to limit costs, while keeping quality of care high.
- Some examples of MCOs you may have heard of health maintenance organizations (HMO’s), preferred provider organizations (PPO), and exclusive provider organization (EPO). Each of these plans have different rules for who you can access services from, how you can get referrals for speciality care, and rates for payment.
- Direct billing (or fee-for-service)= collecting insurance information from someone to bill their insurance company for services that are provided, receiving payments from the insurance company based on rates that are set by type of service (varies depending on insurance)
- Capitated payment = a fixed amount of money per patient per unit of time paid in advance to the healthcare service provided.
- Value-based payments = reimbursement that focuses on how to prevent chronic diseases and hospital visits, aiming for high quality health coordination instead of fee-for-service; this is a value over volume model. The following are types of value-based payments:
-
- Pay for Performance = Working with an insurer to receive a “capitation payment” (i.e. a fixed amount of money per patient per unit of time paid in advance to the healthcare service provider) for a desired outcome.
- Bundled Payment = Capitation payments where insurers pay both a set fee for a patient and pay you the amount needed for the provider to achieve documented improved outcomes for your patient population at a lower cost.
- Shared Savings = Partnering with a Health Home or other entity that has a specific list of people with two or more chronic conditions and agreeing to offer wrap-around services (e.g. care coordination, referrals, health education) as part of a “team approach” to support that individual stay in care and prevent adverse health outcomes.
- Carve-ins/Carve-outs= Terms used to describe how behavioral health and substance use services were included in healthcare plans (“carve-ins”) or how they are excluded from a healthcare plan (“carve-outs”) and paid instead via fee for service by the state and managed by an MCO. Learn more here about Medicaid carve-outs for behavioral health since they vary state-to-state, and here for implementation stories and lessons learned.
- Peer support services= also referred to as recovery support services are designed to offer peer-to-peer support by credentialed workers with lived experience. Services may include coaching, system/care navigators, and assertive community treatment (“ACT teams”) services. Learn more about peer support services here and check out your specific state peer support services here.
